|
Eleanor Dittmer, a resident in the assisted living unit of the Harriett and Ralph Kaplan Estates in Peabody, MA, has a drive-by birthday party in the parking lot of the facility on April 26, 2020. (Photo by Pat Greenhouse/The Boston Globe via Getty Images)
In California, at least 1,434 nursing home residents have died from COVID-19 — 38% of the total fatalities across the state. The actual number is likely higher. Only about 80% of the state's 1,100 licensed nursing facilities are reporting COVID-19 infections or deaths to regulators.
Workers at California nursing homes are often paid "little more than minimum wage." To make ends meet, any nursing home employees end up working at multiple facilities. This has created a concern that workers, especially if they are asymptomatic, are spreading the coronavirus.
Despite the number of deaths, in most facilities, "patients are tested only if they show symptoms or if they choose to be."
The pandemic has also exacerbated existing staffing shortages. Workers are taken out of rotations if they get sick, and others have quit because they are not willing to risk constant exposure to COVID-19 for low wages.
How are nursing homes handling staffing shortages when, during a pandemic, it takes more work than ever to keep residents safe? It's hard to say. Outside visitors have been banned, cutting off seniors from their families and friends.
Nevertheless, as the body count rises, California Governor Gavin Newsom (D) is considering granting nursing homes broad immunity against residents who are suffer injury or death during the pandemic. The request was made by industry groups, including the California Assisted Living Association, to Newsom in a letter last month. The groups have asked Newsom to issue an executive order that contains the following language:
In recognition of these extraordinary and unprecedented circumstances, such facilities… shall be immune from any administrative sanction or criminal or civil liability or claim for any injury, death, or loss alleged to have resulted from any act, omission, or decision made related to providing or arranging services, including but not limited to acts, omissions, or decisions undertaken because of a lack of resources, absent proof by no less than clear and convincing evidence of willful misconduct as measured by a standard of care that incorporates all of the circumstances of the emergency. All state statutes and regulations are hereby waived to the extent necessary to achieve this immunity.
The standard of "willful misconduct" would preclude nearly all legal claims and would allow nursing homes to escape liability, in most cases, even when a resident dies due to the facility's negligence.
"Advocates for older and disabled residents of care facilities, including Senior and Disability Action, California Advocates for Nursing Home Reform, and the Consumer Advocates for RCFE Reform have all objected to the request," KQED, a California NPR affiliate, reported. The advocates argue that nursing homes "already have significant legal protections under law – which were further strengthened when the Trump administration watered down Obama-era policies that had blocked homes from forcing residents to forego their right to sue in favor of arbitration."
The effort to lobby Newsom is part of a multi-million dollar industry lobbying effort that has already persuaded 16 states "to offer facilities some level of immunity for actions in care facilities during declared emergencies related to coronavirus, either through executive order or legislation."
An analysis by New York Assembly Member Ron Kim found that states "without higher liability standards or blanket immunity protection during the COVID-19 pandemic have much lower fatality rates" in nursing homes. Kim is leading the charge to repeal legislation signed by New York Governor Andrew Cuomo (D) in April. That legislation was "drafted and aggressively advocated for" by a lobbying group.
COVID-19 didn't create the problems in nursing homes; it exposed them
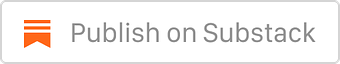
A recent report from the General Accountability Office (GAO) examined "infection prevention and control deficiencies in nursing homes in the years prior to the COVID-19 pandemic." The GAO report found that, between 2013 and 2017, 82% of the nation's 15,000 nursing homes had "an infection prevention and control deficiency cited in one or more years." Almost 10,000 nursing homes were cited for multiple deficiencies over the time period.
These kinds of deficiencies include "situations where nursing home staff did not regularly use proper hand hygiene or failed to implement preventive measures during an infectious disease outbreak, such as isolating sick residents and using masks and other personal protective equipment to control the spread of infection." The GAO report found that "these practices can be critical to preventing the spread of infectious diseases, including COVID-19."
 |
In 2017 alone, 712 of California's 1174 nursing homes were cited "with an infection prevention and control deficiency."
"They killed my dad"
Prior to the pandemic, the failure to control the spread of infections did not typically result in death. Now things have changed.
Last Thursday, the family of a 77-year-old Ricardo Saldana sued Glenhaven Healthcare, located in Glendale, Calfornia. The lawsuit accuses the nursing home "of preventing staff from wearing masks and gloves during the pandemic, downplaying the threat of the virus and withholding information about exposure to COVID-19."
"I’m bringing this case to prevent this from happening to others, and to save lives,” Jackie Saldana, the man's daughter, said. “They killed my dad. They could have prevented this.”
The facility claims, "nursing staff has followed health guidelines put forth by local and federal authorities." But federal inspection reports in recent years "show several deficiencies, including infection control problems." One report in 2019 noted the failure "to ensure that the facility staff performed hand hygiene after touching a potentially contaminated surface or objects and continuing with resident care.”
The national lobbying campaign
Across the country, "at least 28,100 residents and workers have died from the coronavirus at nursing homes and other long-term care facilities." The nursing home industry has had some success in convincing states to provide them with legal immunity. But it is now pressing for national legislation.
The industry "has spent more than $4 million on lobbying over the past year, employing more than a dozen full-time lobbyists." It has also recently contracted with "Brian Ballard, former lobbyist for President Donald Trump, and ex-Mississippi Gov. Haley Barbour, a former Republican National Committee chairman."
The nursing home lobbyists are seeking "a high bar for liability, such as cases of gross negligence." Senator Mitch McConnell (R-KY) and other Republican leaders have said corporate liability protections are an essential component of any future legislation to address the pandemic.
The rise of private equity
The problems at nursing homes have been exacerbated by a surge of investment from private equity firms, which have "poured $5.3 billion into nursing home deals since 2015." Overall, private equity firms own 11% of nursing homes in the United States. A recent study found "private-equity ownership of nursing homes across the U.S. has coincided with cost-cutting, declining quality of care and increasing violations discovered in government inspections."
In the context of a pandemic, even a slight degradation in quality can be deadly. "All it takes is one staff member ignoring standard precautions to expose everybody in a nursing home to dangerous infections,” Michael Connors, an advocate at California Advocates for Nursing Home Reform, said.
Thanks for reading!
 |