| 👉 Peter Attia - The Portfolio to Live Longer (Join Colossus) ❓ Why am I sharing this article? Very interesting podcast from Peter Attia, that connects with the approach we want to have at Alan. I think we need to go deeper into the science of all this. “The name of the game is living longer without chronic disease, not living longer with chronic disease.” ➡️ the objective of Alan. Take a lifetime risk posture. Type 2 diabete is more of a US problem but growing everywhere. The focus should be exercise, nutrition, sleep, stress management. What is hard is to know what advice to give to people, and it is where Alan enters. Power our members to be in charge of their health How do doctors learn about nutrition, exercise? Sleep? Stress management? Is it at medical school? It looks like it isn’t. His stats on exercise are really interesting (to be double checked) “There really is no better way to integrate physical health and emotional health than outdoor exercise.” We should all walk more 🙂 (during 1on1s for example) How to simplify nutrition? There are many ways to get to the result without being obsessive.
The importance of primary prevention: The model today for treating cardiovascular disease is, okay, we treat everybody for secondary prevention. Secondary prevention means you've already had a heart attack or a stroke. The real rub comes in what we think about for primary prevention. How do you treat a person who has not yet had a heart attack or stroke. And the mainstream view on that is, well, we use models that predict risk. We have decent actuary models that predict risk based on lipids, smoking history, blood pressure, family history, et cetera. And we wait until there's a threshold that's crossed to begin treating.
How we manage chronic diseases today: So in the cardiovascular literature, it's typically viewed as about a 5% 10-year risk for a major adverse cardiac event. So if I plug your numbers in, and your 10-year risk comes back at 3%, it is not deemed necessary to put any treatment preventive protocols in place. We know that smoking is causally related to lung cancer. There's no ambiguity about this that smokers are 10x more likely on average to get lung cancer than nonsmokers. When it comes to managing diabetes or cardiovascular disease or other forms of cancer that are not related to smoking or that have other risk factors, we completely fail in that same line of thinking. We don't treat the causal agents, and we don't take an aggressive enough lifetime risk posture.
The underlying risk from type 2 diabetes: So the three are cardiovascular and cerebrovascular disease at #1 leading cause of death; cancer, #2; and neurodegenerative disease, #3, at least in a nonsmoking population because I'm stripping out COPD, chronic obstructive pulmonary disease. But the fourth one is kind of a category I've created from a disease such as type 2 diabetes at one end of the spectrum, but also all the things that are leading up to that. So insulin resistance hyperinsulinemia, nonalcoholic fatty liver disease, which progresses to nonalcoholic steatohepatitis, all the way to type 2 diabetes. Again, if you added up all the death certificates in the country and said how many times does insulin resistance appear on it? The answer is never. No cause of death is insulin resistance. NAFLD is not a cause of death.
Very few people are dying directly as a consequence of type 2 diabetes. But if you have type 2 diabetes, your risk of heart disease, cancer and Alzheimer's disease is approximately 2x that of someone who does not.
What to do: The answer is not just do infinite cancer screening and reduce your risk of cancer or we're just going to treat lipid risk factors and eliminate cardiovascular disease. No, the answer is you have to do all of the above, including addressing metabolic health. And this is where the really unsexy, not terribly interesting word that I hate, lifestyle modification, comes in because we don't really have amazing drugs to do that the way we have drugs to zap lipids or treat hypertension, which, by the way, can also be impacted by those metabolic factors. But this is why exercise, nutrition, sleep, stress management, again, they have the reputation for being so uninteresting because it's like, yes, yes, yes. I know that, I know that, I know that. But it's like no, a, do you understand how much power those things have? And b, do you understand how to dose them? This is the thing, right? I mean every doctor knows exercise is important. We are not trained in what that looks like.
We don't know what advice to give a person. And the same is true with nutrition. They don't really know what to tell people. We certainly don't know what to tell people how to sleep better beyond, if you're having trouble sleeping, here's a suite of medications that can help.
Medicine 3.0: The first is, is the transition to Medicine 3.0, is it necessarily going to have to be driven by health care as the system? Or can it be consumer-driven or patient-driven? So my hypothesis, which I'm happy to be wrong on, is that I actually don't think medicine has to lead the way. I think it can get dragged along the way. In other words, I think enough people can just say, "I'm going to take charge of this. I'm going to be in charge of my own health care. I'm going to be in charge of my Medicine 3.0 approach.
The training of doctors: 80% of what can impact the length and quality of your life, you don't need a doctor for. It's interesting that 20% of that equation is all we learned in medical school and beyond. So when you encounter a doctor who has insight beyond eat less and exercise more, and there are lots of doctors that do have insights beyond that, you have to understand that those insights came to them through their own education and their own process of learning outside of what they learned in medical school or residency.
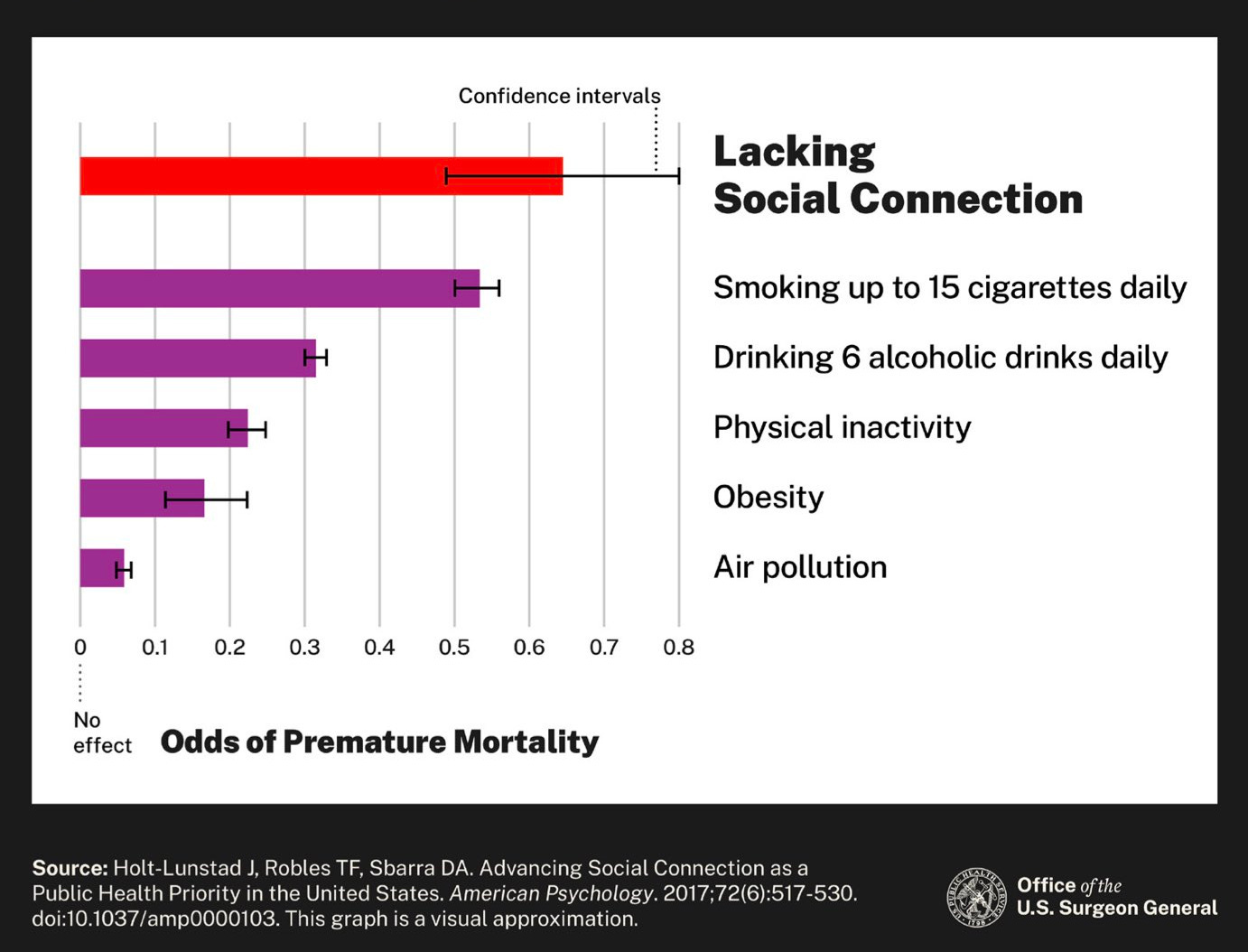
How to approach experiments: If we talk about sleep, nutrition, exercise, pharmacology, we don't have and we will never have high enough quality randomized experiments to test head-to-head all of these interventions. So instead, what we can do is we can look at deficiencies in each of these things and ask the question, what are the hazard ratios associated with those things? And we can also do that by combining other problems. A smoker compared to a nonsmoker has a 40% chance greater death rate in the coming year. Smoking impacts every chronic disease. It's enormously increasing your risk of cardiovascular disease, cerebrovascular disease, Alzheimer's disease and of course, cancer. Type 2 diabetes, again, depends on the study. Directionally speaking, it's about 1.3 to 1.4 is the hazard ratio. So roughly a 30% to 40% increase in all-cause mortality. If you look at hypertension, having high blood pressure, it's about 1.2. So about a 20% increase in all-cause mortality. When you compare top decile to bottom decile for strength, we're talking about hazard ratios of 3, 200% difference. The biggest gap is when you compare the bottom 25% for VO2 max.
The importance of exercise: So when you compare bottom quartile, which is basically people who are never doing any exercise to third quartile, which could be achieved doing 5 to 6 hours of exercise a week, you're talking about a hazard ratio of 2.75, a 175% difference in all-cause mortality. Exercise is indeed the greatest driver, the greatest lever we have at a longer life, but it comes with a caveat, which is it has to be the right kind of exercise. These generic recommendations of just move, just be active, just garden a little bit. No, that's not going to cut it.
Walking outside: This is a very important part of it. There is no phone. I'm not listening to podcasts, audio books or music, and it's just it. All I can hear is the breeze blowing and the wind moving the leaves and things like that. And that's a very important 45 minutes to an hour for me.
His exercise schedule: And so what I'm doing is about 4 hours a week of steady-state Zone 2 cardio, about 30 minutes a week up to 60 minutes a week of higher-intensity cardio, so pushing that VO2 max system, A more practical way to assess that is about the highest level of work you can do while still carrying out a conversation, albeit difficult. So if you can't carry out a conversation, you're out of Zone 2, you're into Zone 3. If you can speak, but it's easy, you're in Zone 1. So Zone 2, especially the upper end of Zone 2 is, I did a Zone 2 work out today, if my wife -- and I'm doing it on a stationary bike, if my wife comes in and starts talking to me, I can talk to her, I just don't really want to.
About 6 hours a week of strength training that split mostly equally between upper and lower body. And then rucking; probably 3 to 4 hours a week of rucking. I am an advocate of doing it early. I do find that compliance is much easier if it's done before you start work then after work. And I also think it sets your brain up better for the day. So part of that is just developing a habit around doing something. And then before you know it, it actually becomes pretty automatic.
Sleep: Nutrition: Once you're in that zone of being adequately nourished, it's far more important to be focusing on metabolic health and lean mass than to be thinking about the subtle nuances of, well, how much fruit should you eat. If you look at the absolute battles that people have over social media with respect to this diet versus that diet and what about being vegan, what about being paleo, and it's like, it might not actually matter as much as you guys think. Are you in energy balance? Are you metabolically healthy? Are you getting enough protein? After that, I almost joke that I didn't want to write the 2 chapters on nutrition because it creates so much substrate for people to argue about things. And what I really want to say is like those are the 3 questions that matter most. And the rest is just tactics and strategy around what to do. And of course, I go into all those things. How do you use dietary restriction, time restriction, chloric restriction to address the crisis of overabundance, which we have. So most people are over nourished, and I don't think there's some magic around how you fix that. The operationalizing of it is hard, but the strategy is really simple. You can calorie restrict, dietary restrict or time restrict, each one has advantages, each one has disadvantages. They're not mutually exclusive, but they are collectively exhaustive. Try the one that works for you, if you fail, go try another one. What I'm trying to get away from is kind of the dogmatic view that there is a right way.
👉 US Surgeon General’s Report on the Loneliness Epidemic (The Split) ❓ Why am I sharing this article?
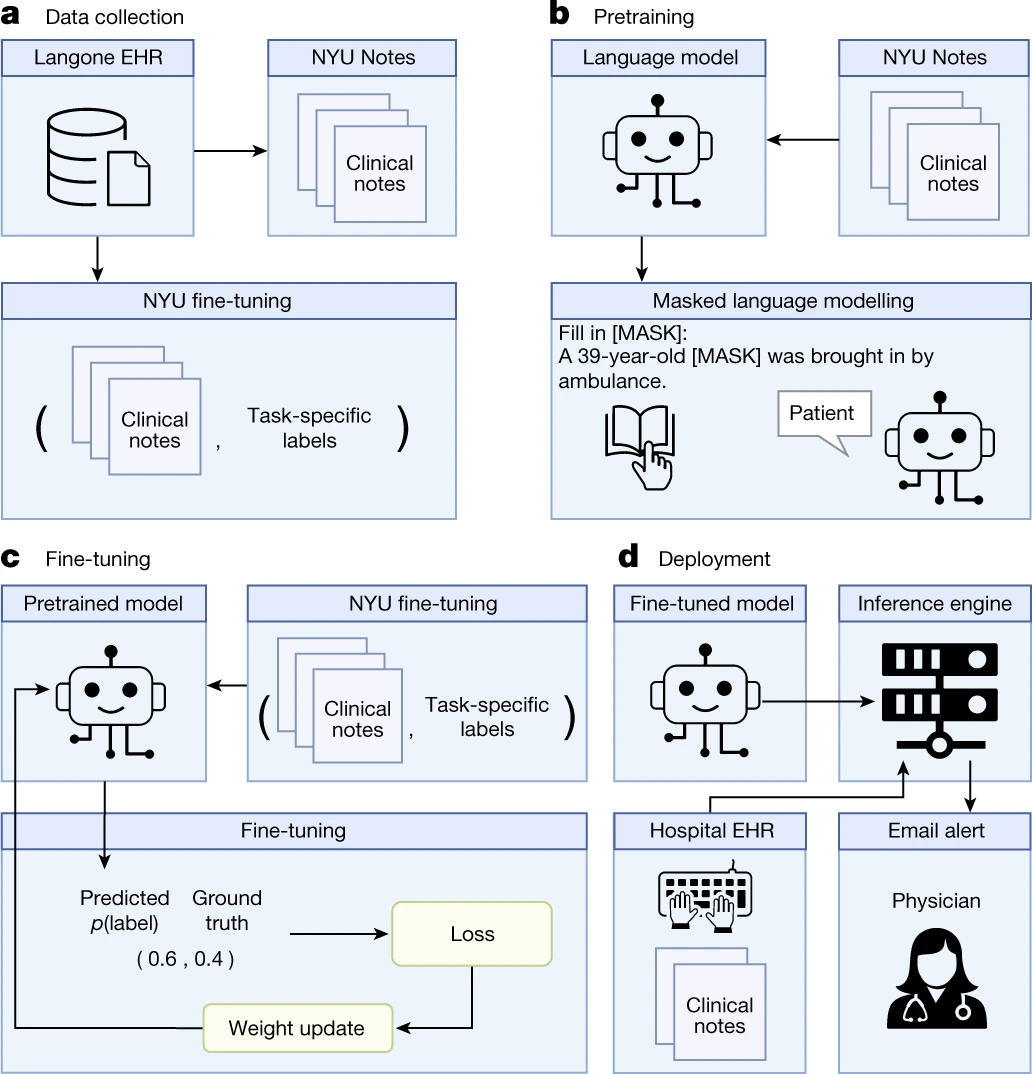
👉 Health system-scale language models are all-purpose prediction engines (Nature) ❓ Why am I sharing this article? Existing structured data-based clinical predictive models have limited use in everyday practice owing to complexity in data processing, as well as model development and deployment. Train a large language model for medical language (NYUTron) and subsequently fine-tune it across a wide range of clinical and operational predictive tasks. We evaluated our approach within our health system for five such tasks: 30-day all-cause readmission prediction, in-hospital mortality prediction, comorbidity index prediction, length of stay prediction, and insurance denial prediction. We show that NYUTron has an area under the curve (AUC) of 78.7–94.9%, with an improvement of 5.36–14.7% in the AUC compared with traditional models.
Fig. 1 | Overview of the language model-based approach for clinical prediction. a, We queried the NYU Langone EHR for two types of datasets. The pretraining dataset, NYU Notes, contains 10 years of inpatient clinical notes (387,144 patients, 4.1 billion words). There are five fine-tuning datasets. Each contains 1–10 years of inpatient clinical notes (55,791–413,845 patients, 51–87 million words) with task-specific labels (2–4 classes). b, We pretrained a 109 million-parameter BERT-like LLM, termed NYUTron, on the entire EHR using an MLM task to create a pretrained model for medical language contained within the EHR. c, We subsequently fine-tuned the pretrained model on specific tasks (for example, 30-day all-cause readmission prediction) and validated it on held-out retrospective data. d, Lastly, the fine-tuned model was compressed into an accelerated format and loaded into an inference engine, which interfaces with the NYU Langone EHR to read discharge notes when they are signed by treating physicians.
👉 Hippocratic is building a large language model for healthcare (TechCrunch+) ❓ Why am I sharing this article? In Hippocratic’s technology, a text-generating model tuned specifically for healthcare applications. Shah emphasized that Hippocratic isn’t focused on diagnosing. Rather, he says, the tech — which is consumer-facing — is aimed at use cases like explaining benefits and billing, providing dietary advice and medication reminders, answering pre-op questions, onboarding patients and delivering “negative” test results that indicate nothing’s wrong.
Hippocratic’s benchmark results on a range of medical exams. Image Credits: Hippocratic But Shah claims that Hippocratic’s AI outperforms leading language models including GPT-4 and Claude on over 100 healthcare certifications, including the NCLEX-RN for nursing, the American Board of Urology exam and the registered dietitian exam. To evaluate bedside manner, Hippocratic designed a benchmark to test the model for signs of humanism, if you will — things like “showing empathy” and “taking a personal interest in a patient’s life.” The company isn’t releasing details on its partners or customers, preferring instead to keep the focus on the funding. The model isn’t even available at present — nor information about what data it was trained on, or what data it might be trained on in the future. (Hippocratic would only say that it’ll use “de-identified” data for the model training.) rivals like Truveta and Latent
👉 16 Healthcare Companies That Already Integrated ChatGPT: Infographic (The Medical Futurist) ❓ Why am I sharing this article?
👉 AI chatbot K Health picks up $59M in fresh funding, inks partnership with Cedars-Sinai (Fierce Healthcare) ❓ Why am I sharing this article? How they accessed data to train their models. Their technology is likely outdated given LLMs but they still have access to the datasets, which is great.
Product & numbers: Launched in 2016 and rolled out into the U.S. market in 2018, K Health developed a chat function that uses artificial intelligence to suggest potential diagnoses for consumers who enter symptoms and also takes into account the user's medical history, age and gender. Its platform sifts through the data of millions of patients and suggests a medical condition and will connect patients with a doctor or nurse, if needed. Ten million people have interacted with K Health’s AI, and 3.1 million patients in 48 states have completed a chat with a doctor or nurse visit via K Health, CEO and co-founder Allon Bloch told Forbes. Along with investing in K Health, Cedars-Sinai also inked a partnership with the digital health company to use its technology for virtual urgent and primary care services, Forbes reported in an exclusive interview about the funding round and the partnership. Forbes pegs the startup's valuation at $800 million. K Health had a reported valuation of $1.5 billion in January 2021, at the height of the digital health boom.
Datasets: Quality:
👉 Talkspace posts narrower loss as B2B revenue increases (Mobi Health News) ❓ Why am I sharing this article? The teletherapy company reported $33.3 million in revenue compared with $30.2 million in the prior-year period. It noted a 71% increase in its B2B revenue year-over-year and 40% decline in its consumer revenue.
👉 Telehealth giant Amwell posts nearly $400M loss in Q1 (Mobi Health News) ❓ Why am I sharing this article? Schoenberg said the platform can embed third-party tools, "much like an app store." He pointed to the company's partnership with chronic condition management company DarioHealth (https://www.mobihealthnews.com/news/amwellpartners-dariohealth-offer-digital-cardiometabolichealth-program) as an example.
👉 How Providence, Northwell are tapping into digital solutions to support women's health and boost worker retention (Fierce Health Care) ❓ Why am I sharing this article? One in four women who experience symptoms of menopause considering early retirement “When we first asked the question of the workforce an overwhelming response from over 900 employees said menopause was top of mind for them,” Santo told Fierce Healthcare. “We got the voice of the patient really early in the process, and that's reflected in the product that we built.” Of women experiencing menopause symptoms, 73% are left untreated for the 10-to-15-year menopause journey.
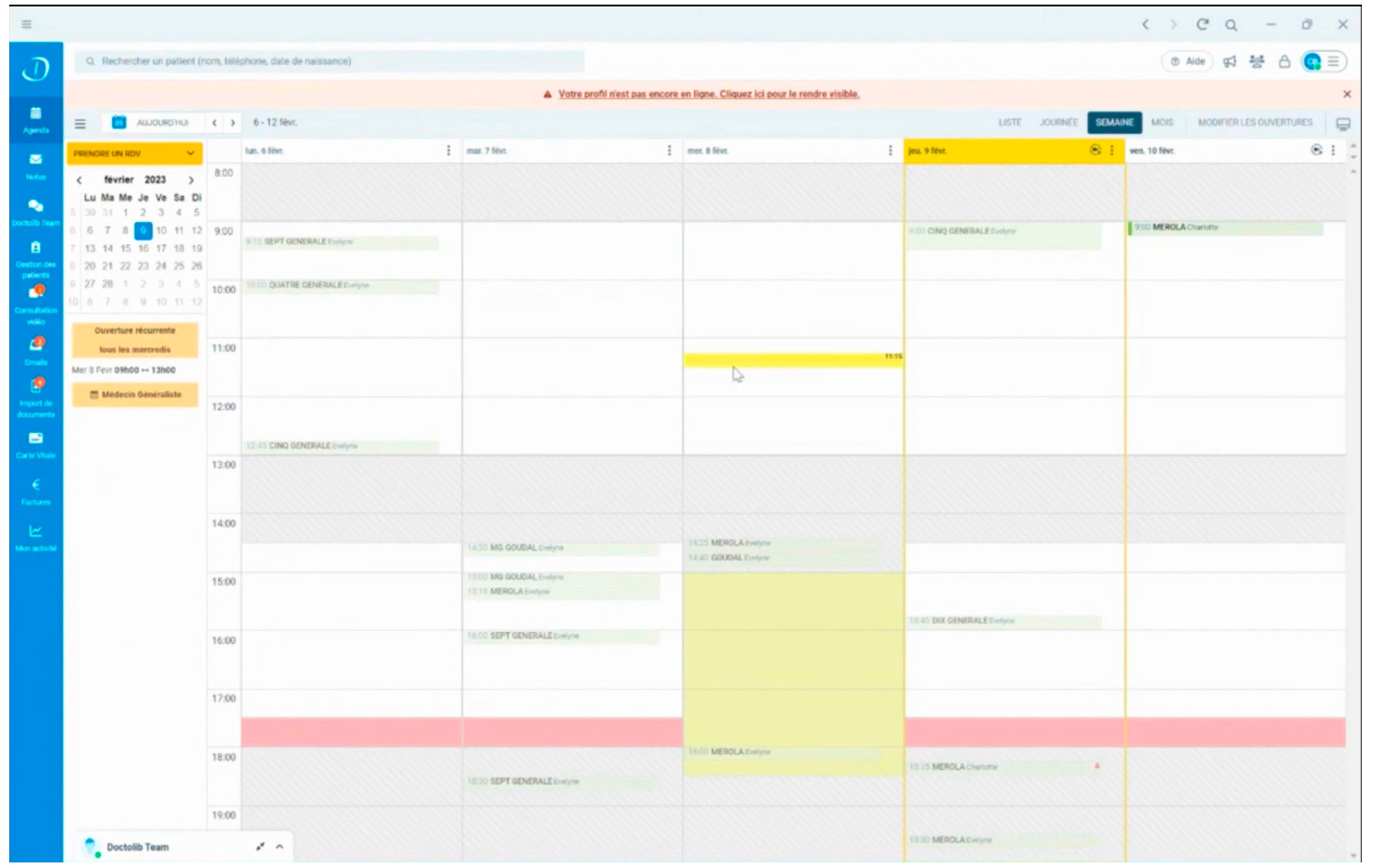
👉 Doctolib - The All-In-One Solution for Independent Healthcare Professionals (Overlooked by Alexandre Dewez) ❓ Why am I sharing this article? Doctolib is trying to upsell more services to doctors (EHR, telemedicine, messaging between doctors, booking) While they are big in terms of healthcare professionals, they are not profitable yet They connected with all the EHRs on the market which is useful, and well done! I didn’t know they had a Carte Vitale player.
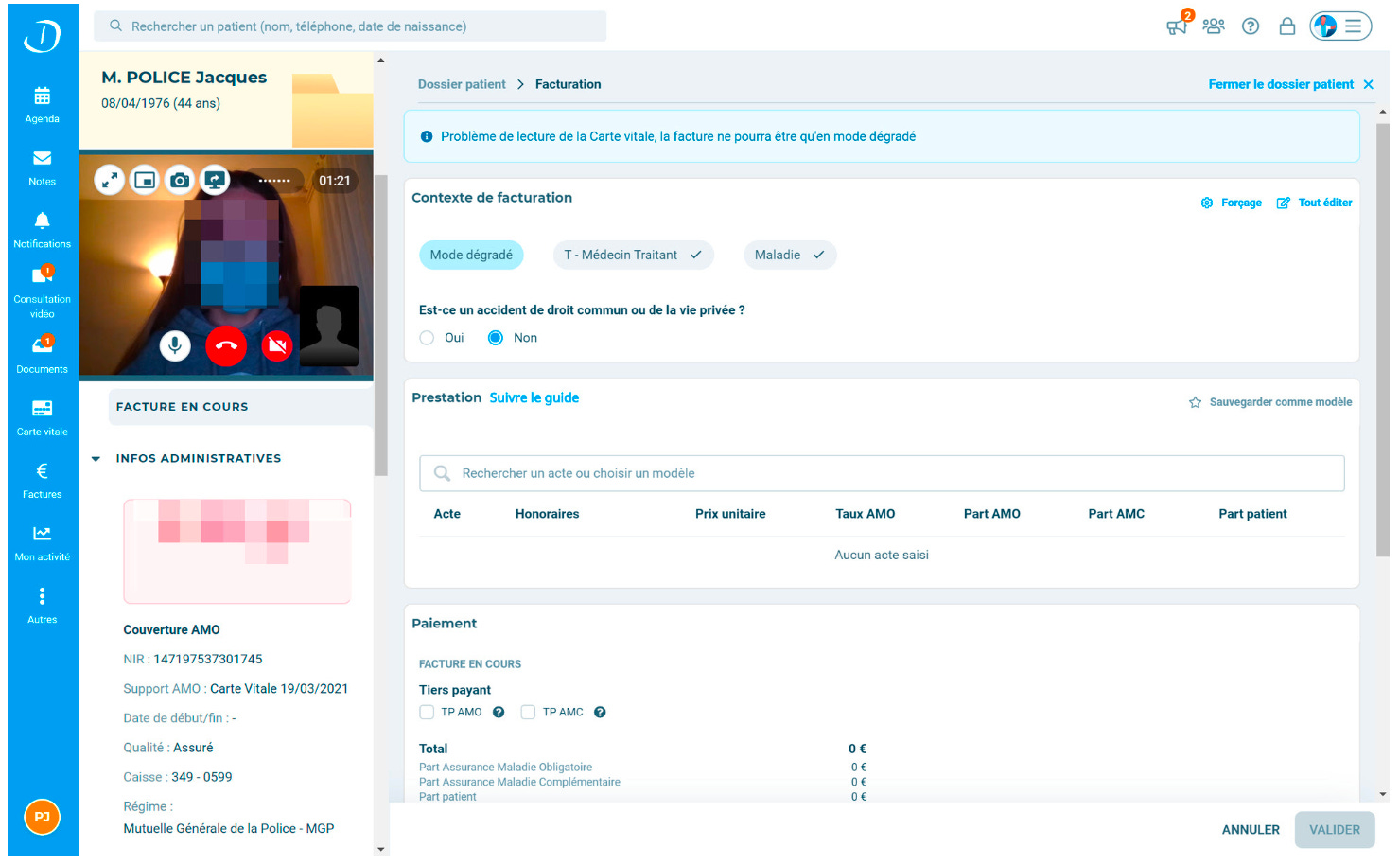
Product overview: With Covid, Doctolib started to expand its product suite to become an all-in-one solution for healthcare professionals with an EHR, a telemedicine platform and a messaging app on top of its initial booking management system. Product: Doctolib offers 6 main products which are fully interconnected: (i) Doctolib Patient, (ii) Doctolib Médecin, (iii) Doctolib Team, (iv) Doctolib Téléconsultation, (v) Doctolib Lecteur and (vi) Doctolib Hôpital. On the product side, it launched its EHR called Doctolib Médecin in March 2021 and a free messaging app for healthcare professionals called Doctolib Teams in March 2022. Doctolib Patient was Doctolib’s initial product. It’s a booming management system for doctors. It has three main benefits: (i) it saves doctors one hour and thirty minutes per week in administrative tasks, (ii) it reduces missed appointments by 60% and (iii) it increases doctors’ revenues by attracting new patients as Doctolib attracts 70 million patients every month on its website.
Doctors can also use Doctolib Patient to communicate with their patients and share documents like prescriptions. Doctolib Patient is connected with all the EHRs on the market. Doctolib Médecin - The Electronic Health Records. It offers: (i) patient management with all the medical information and historical records, (ii) document management to reduce manual entry or double entry, (iii) a consultation space to be more efficient while you treat patients, (iv) invoicing with automatic transmission to the French Social Security which is a State organism reimbursing some medical costs. Doctolib Médecin has industry specific features that are hard to replicate for horizontal products such as pre-filled templates based on the symptoms observed by the doctor, a connection with a drugs library to give out a prescription, AI to identify from emails received a patient conditions and the nature of attached documents and the ability to directly send invoices to be reimbursed. It’s a €135 monthly SaaS that doctors will pay on top of Doctolib Patient.
M&A: Numbers: Today, Doctolib has over 340K healthcare professionals using Doctolib Agenda, 5K using Doctolib Médecin and 70 million patients accounts in France, Germany and Italy. It added 40K healthcare professionals in 2022 (13% YoY growth) and 100K healthcare professionals in 2021 (50% YoY growth). In 2022, Doctolib’s growth of healthcare professionals suffered from its decision to remove non regulated healthcare professionals from its platform (5.7K customers removed). A €139 monthly SaaS fee paid by doctors
Hospitals: TAM: Sales:
👉 Apple unveils watchOS 10 with new features for mental health, vision health (Mobi Health News) ❓ Why am I sharing this article? The watchOS 10 will allow users to log their emotions and daily moods via the Mindfulness app. Users will be able to turn the Digital Crown to select a shape to describe and track their feelings. Another aspect of the new watchOS focuses on vision health, allowing users to measure the amount of time spent outdoors, which the company says can contribute to one's physical and mental health, but also raise the risk of nearsightedness with more sun exposure. The watch will also include an addition to the medications app, where follow-up reminders can be sent 30 minutes after the scheduled time users were supposed to log a medication.
It’s already over! Please share JC’s Newsletter with your friends, and subscribe 👇 Let’s talk about this together on LinkedIn or on Twitter. Have a good week! | |